Imagine a medical emergency where a blood clot travels to your lungs, blocking essential oxygen flow—this is pulmonary embolism, a condition that affects up to 900,000 Americans each year and causes as many as 100,000 deaths. Pulmonary embolism (PE) represents one of the most serious cardiovascular emergencies, yet many people don't recognize its symptoms until it's too late. Understanding how this condition develops, who's at risk, and what treatments are available could literally save your life or the life of someone you love.
How Pulmonary Embolism Happens: The Journey of a Blood Clot
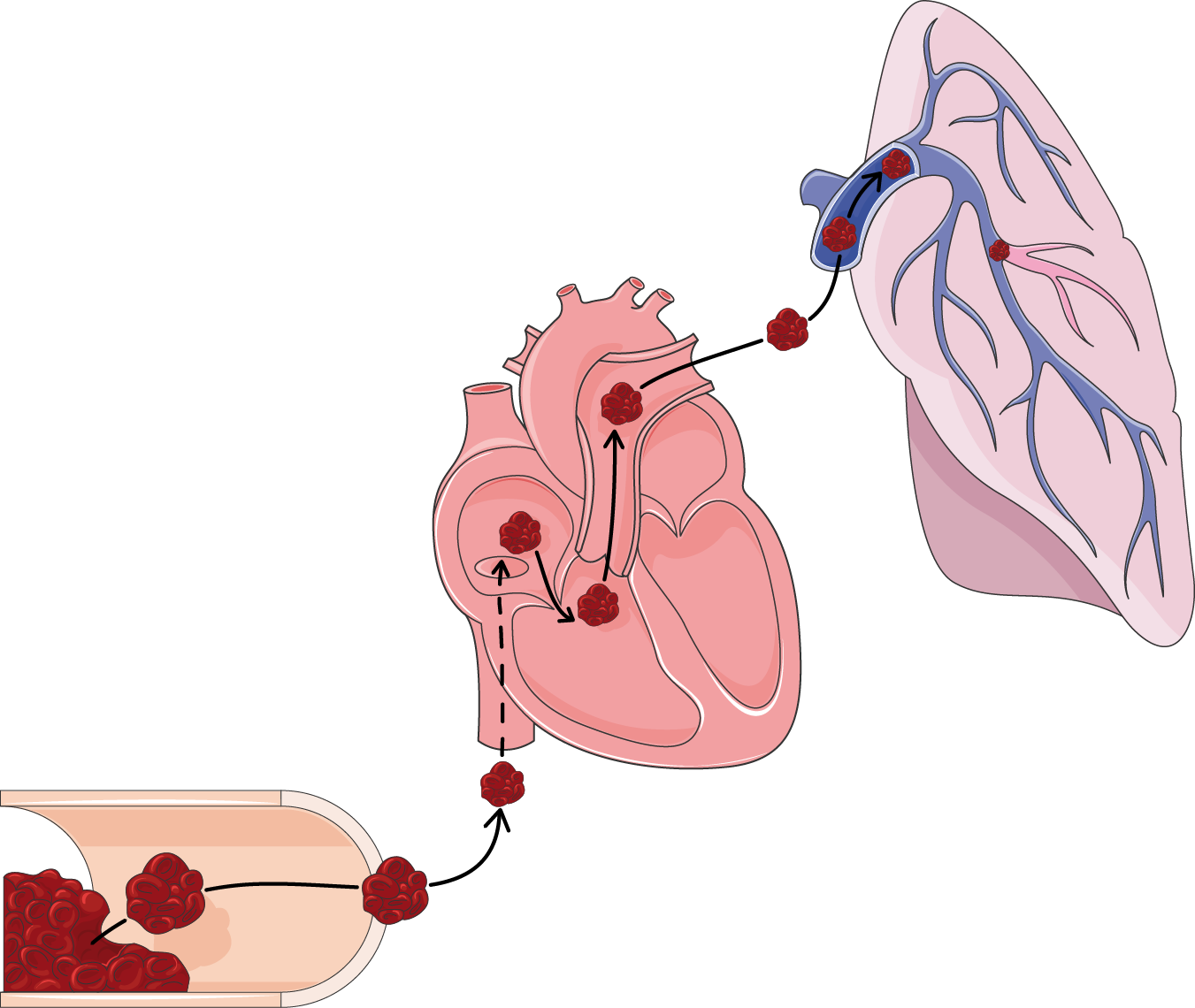
Pulmonary embolism occurs when a blood clot, known as an embolus, travels through the bloodstream and lodges in one of the pulmonary arteries that supply blood to the lungs. In approximately 90% of cases, these clots originate as deep vein thrombosis (DVT) in the legs or pelvic veins. When part of this clot breaks free, it travels through the right side of the heart and into the pulmonary circulation, where it can completely or partially block blood flow to lung tissue.
The process follows Virchow's triad—three factors that contribute to blood clot formation: venous stasis (reduced blood flow), endothelial injury (damage to blood vessel walls), and hypercoagulability (increased blood clotting tendency). Common triggers include prolonged immobility during long flights or hospital stays, surgical procedures (especially orthopedic surgeries), trauma, cancer, pregnancy, and certain medications like hormonal contraceptives.
Recognizing the Warning Signs: Symptoms You Should Never Ignore
The symptoms of pulmonary embolism can vary dramatically depending on the size of the clot and how much of the lung is affected. The most common symptom is sudden shortness of breath that occurs at rest or with minimal exertion. This is often accompanied by sharp, stabbing chest pain that worsens with deep breathing, coughing, or bending over—a symptom known as pleuritic chest pain.
Other warning signs include rapid breathing, a fast heart rate (tachycardia), coughing up blood (hemoptysis), lightheadedness, fainting (syncope), and in severe cases, signs of shock such as low blood pressure and bluish discoloration of the skin (cyanosis). What makes PE particularly dangerous is that in about 25% of cases, sudden death is the first and only symptom, highlighting the critical importance of early recognition and intervention.
Who's at Risk? Understanding Your Vulnerability
Certain factors significantly increase the risk of developing pulmonary embolism. These include recent surgery (especially hip or knee replacement), hospitalization with prolonged bed rest, active cancer or cancer treatment, pregnancy and the postpartum period, use of estrogen-containing medications (birth control pills or hormone replacement therapy), and inherited clotting disorders like Factor V Leiden.
Additional risk factors include obesity, smoking, age over 40, a personal or family history of blood clots, chronic medical conditions like heart failure or inflammatory bowel disease, and long periods of immobility such as during extended travel. The CDC notes that more than one-third of VTE cases are related to recent hospitalization, making hospital-associated clots a major public health concern.
Diagnosing the Silent Threat: How Doctors Detect Pulmonary Embolism
Diagnosing pulmonary embolism requires a combination of clinical assessment, blood tests, and imaging studies. Physicians typically begin with a Wells score or Geneva score—clinical prediction rules that estimate the probability of PE based on symptoms, risk factors, and physical findings. Blood tests measure D-dimer levels, a protein fragment present when blood clots break down; elevated levels suggest possible clot formation.
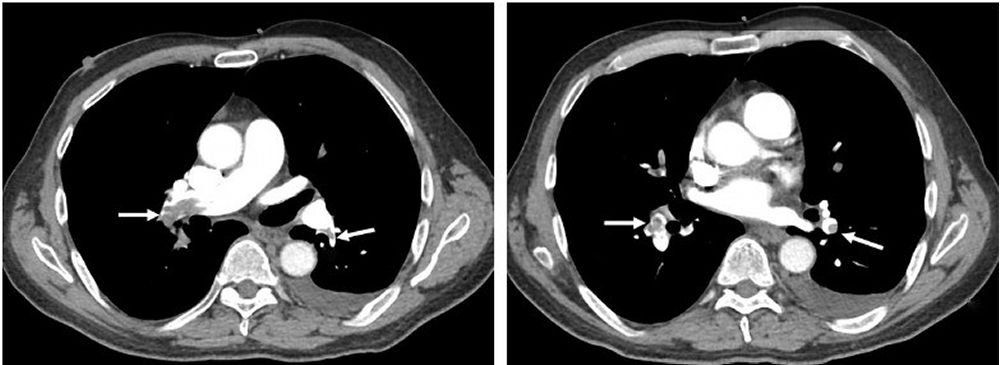
When suspicion is high, imaging tests provide definitive diagnosis. CT pulmonary angiography (CTPA) has become the gold standard, offering detailed images of pulmonary arteries to identify blockages. Ventilation-perfusion (V/Q) scanning, which compares air flow and blood flow in the lungs, is used when CT scanning isn't possible. Doppler ultrasound of the legs can detect DVT, while echocardiography may show signs of right heart strain caused by large pulmonary emboli.
Treatment Options: From Blood Thinners to Advanced Procedures
Treatment for pulmonary embolism depends on the severity of the condition. For most patients, anticoagulant medications (blood thinners) form the foundation of therapy. These include injectable medications like heparin or enoxaparin, followed by oral agents such as warfarin or direct oral anticoagulants (DOACs) like rivaroxaban or apixaban. These medications don't dissolve existing clots but prevent new ones from forming while the body's natural systems break down the blockage.
For life-threatening cases with massive PE causing shock or low blood pressure, more aggressive treatments are necessary. Thrombolytic therapy ("clot-busting" drugs like alteplase) can rapidly dissolve clots but carries significant bleeding risks. Catheter-directed thrombectomy uses minimally invasive techniques to mechanically remove or break up clots, while surgical embolectomy involves open-heart surgery to remove large, central emboli.
Life After Pulmonary Embolism: Recovery and Long-Term Management
Recovery from pulmonary embolism varies depending on the clot size, treatment response, and underlying health. Most patients require 3-6 months of anticoagulant therapy, while those with recurrent clots or ongoing risk factors may need lifelong treatment. During recovery, patients may experience decreased exercise tolerance, breathlessness, and fatigue—a condition sometimes called post-PE syndrome.
Approximately 2-4% of survivors develop chronic thromboembolic pulmonary hypertension (CTEPH), a serious complication where persistent clots cause high blood pressure in the lung arteries. Regular follow-up with healthcare providers, pulmonary rehabilitation programs, and lifestyle modifications are essential components of long-term management. Newer treatments like pulmonary endarterectomy and balloon pulmonary angioplasty now offer hope for CTEPH patients who previously had limited options.
Prevention Strategies: Reducing Your Risk of Blood Clots
Preventing pulmonary embolism begins with awareness of personal risk factors and proactive measures. For hospitalized patients, mechanical prophylaxis with intermittent pneumatic compression devices and graduated compression stockings reduces venous stasis. Pharmacological prophylaxis with low-dose anticoagulants is standard for most surgical patients and many medical inpatients.
For the general population, maintaining a healthy weight, staying physically active, avoiding prolonged immobility, and discussing medication risks with healthcare providers are key preventive steps. During long trips, frequent movement, calf exercises, and proper hydration can reduce travel-related thrombosis risk. Individuals with a history of blood clots should work closely with their healthcare team to determine appropriate duration of anticoagulation and monitoring strategies.
Key Takeaways About Pulmonary Embolism
Pulmonary embolism remains a major public health concern with significant mortality, but increased awareness and advances in diagnosis and treatment have improved outcomes. Remember these essential points: PE often starts as a leg clot that travels to the lungs; symptoms like sudden shortness of breath and chest pain require immediate medical attention; prompt treatment with anticoagulants saves lives; and preventive measures are particularly important during hospitalization, surgery, pregnancy, and prolonged immobility. By understanding this condition and its risk factors, individuals can take proactive steps to protect their health and recognize warning signs that demand emergency care.